At the University of Toronto, scientists have come up with a new theory to describe how nanoparticles enter and exit the tumors they are intended to treat. This possibly rewrites the knowledge of cancer nanomedicine that has directed research for almost four decades.
 Schematic of nanoparticle exit via the intratumoral lymphatic vessels. Nanoparticles in the tumor move toward the lymphatic vessel, cross the vessel wall, and drain into the vessel lumen. Image Credit: Nguyen, L.N.M., Lin, Z.P., Sindhwani, S. et al.
Schematic of nanoparticle exit via the intratumoral lymphatic vessels. Nanoparticles in the tumor move toward the lymphatic vessel, cross the vessel wall, and drain into the vessel lumen. Image Credit: Nguyen, L.N.M., Lin, Z.P., Sindhwani, S. et al.
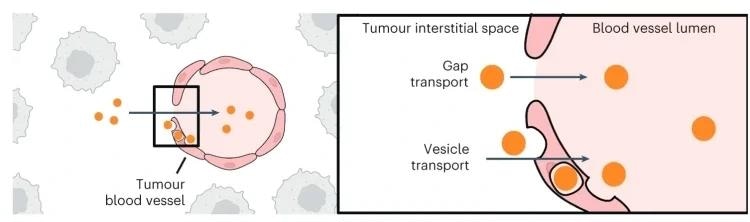
The Enhanced Permeability and Retention (EPR) effect, an idea largely unquestioned since the mid-1980s, posits that nanoparticles enter a tumor from the bloodstream via gaps between the endothelial cells that line its blood vessels–and further turn out to be trapped in the tumor as a result of dysfunctional lymphatic vessels.
The retention aspect of the EPR theory is contingent on the lymphatic vessel cavity being too small for nanoparticles to exit, thereby helping nanoparticles that carry cancer-fighting drugs to stay in the tumors.
Matthew Nguyen, Ph.D. Student, Institute of Biomedical Engineering, University of Toronto
Matthew Nguyen is also associated with the Donnelly Centre for Cellular and Biomolecular Research.
Nguyen added, “But we found around 45% of nanoparticles that accumulate in tumors will end up exiting them.”
Nguyen, who is a member of the lab of Professor Warren Chan, is the lead author of a new study that challenges a long-standing theory, recently published in the journal Nature Materials.
The study outcomes of researchers help describe why treatments based on the EPR effect are a failure in clinical trials, building on the earlier study from the Chan laboratory that revealed that below 1% of nanoparticles reach tumors.
The scientists discovered that, in opposition to the EPR effect, nanoparticles could leave tumors via their lymphatic vessels.
The exit method for a nanoparticle relies on its size; bigger ones (50 to 100 nm wide) are more likely to exit lymphatic vessels in the tumors, and smaller ones (up to 15 nm wide) are more likely to leave through lymphatic vessels encircling the tumors.
In exceptional cases, nanoparticles will depart through blood vessels.
Nanoparticle exit from tumors happens via spaces in the lymphatic vessel walls and transport vesicles that carry them through these walls. The scientists displayed that nanoparticles will re-enter the bloodstream after lymphatic drainage. They hypothesized that such nanoparticles will eventually return to the tumor for one more chance to treat it.
Denying the EPR effect was no simple feat. The Chan laboratory spent almost years working to comprehend why nanoparticles do not house tumors efficiently.
Before this study was performed, the laboratory concentrated on how nanoparticles enter the tumors. By doing this and other studies, the lab came up with a competing theory to the EPR effect, known as the Active Transport and Retention (ATR) principle.
Nguyen believed that the field of nanomedicine has developed since the publication of the nanoparticle entry study in 2020.
We got more pushback from other researchers on that study compared to this one. People have started to accept that the EPR effect is flawed.
Matthew Nguyen, Ph.D. Student, Institute of Biomedical Engineering, University of Toronto
With almost half of the accumulated nanoparticles exiting tumors, mostly via lymphatic vessels, future research can tackle this problem through nanoparticle treatments that avoid lymphatic drainage.
We are excited to have a better understanding of the nanoparticle tumor delivery process. The results of these fundamental studies on nanoparticle entry and exit will be important for engineering nanoparticles to treat cancer.
Warren Chan, Professor, University of Toronto
The study’s outcomes, if employed across the field of cancer nanomedicine, promise a new direction to enhance the knowledge of how nanoparticles could be utilized to treat tumors.
“Trying to translate cancer nanomedicine to the clinic is like a working with a black box – some drugs work, some don’t, and it’s difficult to know why,” stated Gang Zheng, Associate Research Director at the Princess Margaret Cancer Center and Professor of Medical Biophysics in U of T’s Temerty Faculty of Medicine who was not involved in the study.
Zheng added, “Chan’s dedication to better understanding the mechanisms of nanoparticle uptake and exit is shining light on these processes to help make our translation efforts more efficient and successful.”
The study was financially supported by the Canadian Cancer Society, the Canadian Institutes of Health Research, NanoMedicines Innovation Network, and the Canada Research Chairs program.
Journal Reference:
Nguyen, L. N. M., et al. (2023) The exit of nanoparticles from solid tumors. Nature Materials. doi.org/10.1038/s41563-023-01630-0.
Source: https://www.utoronto.ca/