Feb 10 2011
Microsponges derived from seaweed may help diagnose heart disease, cancers, HIV and other diseases quickly and at far lower cost than current clinical methods.
The microsponges are an essential component of Rice University's Programmable Bio-Nano-Chip (PBNC) and the focus of a new paper in the journal Small.
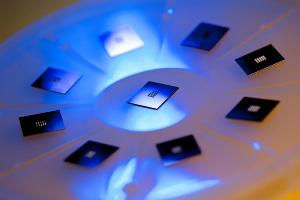 At the heart of Rice University's Programmable Bio-Nano-Chip is a grid that contains microsponges, tiny agarose beads programmed to capture biomarkers. The biomarkers help clinicians detect signs of disease in patients.
At the heart of Rice University's Programmable Bio-Nano-Chip is a grid that contains microsponges, tiny agarose beads programmed to capture biomarkers. The biomarkers help clinicians detect signs of disease in patients.
The paper by John McDevitt, the Brown-Wiess Professor in Bioengineering and Chemistry, and his colleagues at Rice's BioScience Research Collaborative views the inner workings of PBNCs, which McDevitt envisions as a mainstream medical diagnostic tool.
PBNCs to diagnose a variety of diseases are currently the focus of six human clinical trials. McDevitt will discuss their development at the annual meeting of the American Association for the Advancement of Science (AAAS) in Washington, D.C., Feb. 17-21.
PBNCs capture biomarkers -- molecules that offer information about a person's health -- found in blood, saliva and other bodily fluids. The biomarkers are sequestered in tiny sponges set into an array of inverted pyramid-shaped funnels in the microprocessor heart of the credit card-sized PBNC.
When a fluid sample is put into the disposable device, microfluidic channels direct it to the sponges, which are infused with antibodies that detect and capture specific biomarkers. Once captured, they can be analyzed within minutes with a sophisticated microscope and computer built into a portable, toaster-sized reader.
The biomarker capture process is the subject of the Small paper. The microsponges are 280-micrometer beads of agarose, a cheap, common, lab-friendly material derived from seaweed and often used as a matrix for growing live cells or capturing proteins.
The beauty of agarose is its ability to capture a wide range of targets from relatively huge protein biomarkers to tiny drug metabolites. In the lab, agarose starts as a powder, like Jell-O. When mixed with hot water, it can be formed into gels or solids of any size. The size of the pores and channels in agarose can be tuned down to the nanoscale.
The challenge, McDevitt said, was defining a new concept to quickly and efficiently capture and detect biomarkers within a microfluidic circuit. The solution developed at Rice is a network of microsponges with tailored pore sizes and nano-nets of agarose fibers. The sponge-like quality allows a lot of fluid to be processed quickly, while the nano-net provides a huge surface area that can be used to generate optical signals 1,000 times greater than conventional refrigerator-sized devices. The mini-sensor ensembles, he said, pack maximum punch.
The team found that agarose beads with a diameter of about 280 micrometers are ideal for real-world applications and can be mass-produced in a cost-effective way. These agarose beads retain their efficiency at capturing biomarkers, are easy to handle and don't require specialized optics to see.
McDevitt and his colleagues tested beads with pores up to 620 nanometers and down to 45 nanometers wide. (A sheet of paper is about 100,000 nanometers thick.) Pores near 140 nanometers proved best at letting proteins infuse the beads' internal nano-nets quickly, a characteristic that enables PBNCs to test for disease in less than 15 minutes.
The team reported on experiments using two biomarkers, carcinoembryonic antigens and Interleukin-1 beta proteins (and matching antibodies for both), purchased by the lab. After soaking the beads in the antibody solutions, the researchers tested their ability to recognize and capture their matching biomarkers. In the best cases, they showed near-total efficiency (99.5 percent) in the detection of bead-bound biomarkers.
McDevitt has expected for some time that a three-dimensional bead had greater potential to capture and hold biomarkers than the standard for such tests, the enzyme-linked immunosorbent assay (ELISA) technique. ELISA analyses fluids placed in an array of 6.5-millimeter wells that have a layer of biomarker capture material spread out at the bottom. Getting results through ELISA requires a lab full of equipment, he said.
"The amount of optical signal you get usually depends on the thickness of a sample," McDevitt said. "Water, for example, looks clear in a small glass, but is blue in an ocean or a lake. Most modern clinical devices read signals from samples in flat or curved surfaces, which is like trying to see the blue color of water in a glass. It's very difficult."
By comparison, PBNCs give the researchers an ocean of information. "We create an ultrahigh-surface-area microsponge that collects a large amount of material," he said. "The sponge is like a jellyfish with tentacles that capture the biomarkers."
The agarose bead is engineered to become invisible in water. "That makes it an ideal environment to capture biomarkers, because the matrix doesn't get in the way of visualizing the contents. This is a nice use of novel biomaterials that are cheap as dirt, yet yield powerful performance," McDevitt said.
According to previous studies, only a fraction -- less than 10 percent -- of capture antibodies in the "gold standard" ELISA arrays are still active by the time a test begins. By comparison, nearly all of the antibodies in the agarose beads retain their ability to detect and capture biomarkers, McDevitt said.
Ultimately, he said, PBNCs will enable rapid, cost-effective diagnostic tests for patients who are ailing, whether they're in an emergency room, in an ambulance or even while being treated in their own homes. Even better, the chips may someday allow for quick and easy testing of the healthy to look for early warning signs of disease.
Co-authors of the paper included first author Jesse Jokerst, a National Institutes of Health postdoctoral fellow at Stanford University; postdoctoral students James Camp, Jorge Wong, Alexis Lennart, Amanda Pollard and Yanjie Zhou, all of the departments of Chemistry and Biochemistry at the University of Texas at Austin; Mehnaaz Ali, an assistant professor of chemistry at Xavier University; and from the McDevitt Lab at Rice, Pierre Floriano, director of microfluidics and image and data analysis; Nicolaos Christodoulides, director of assay development; research scientist Glennon Simmons and graduate student Jie Chou.
The National Institutes of Health, through the National Institute of Dental and Craniofacial Research, funded the research.
Source: http://media.rice.edu/