Cancer is one of the leading causes of death worldwide. To improve cancer treatment efficacy and reduce side effects, scientists have developed several tumor-targeting, carbon, lipid, liposome-based, and cell membrane-coated nanoparticles for cancer applications.
But how do these nanoparticles efficiently target tumors and improve survival outcomes?
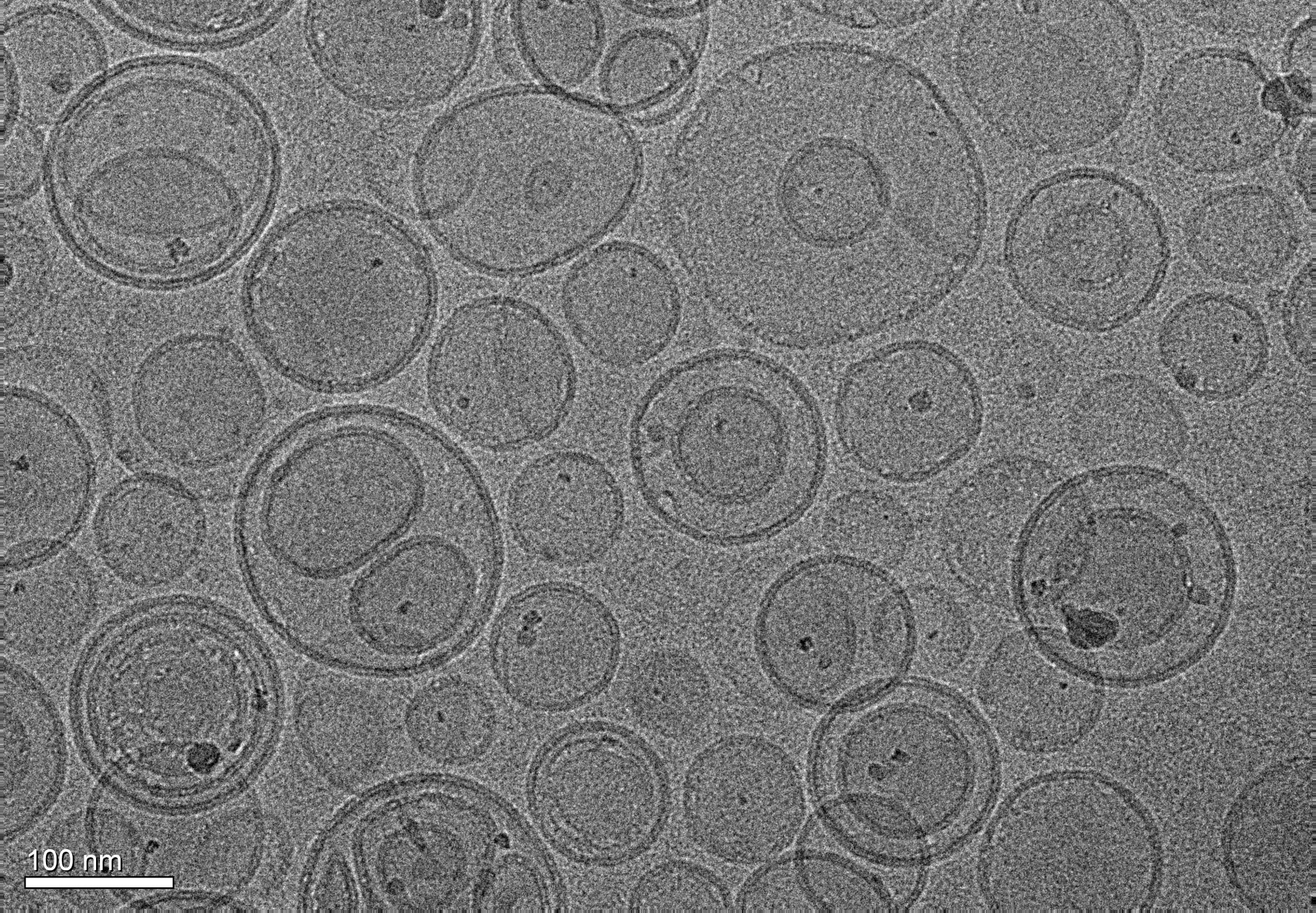
Image Credit: Dr. Pierre-Alain Burnouf/Shutterstock.com
Nanomedicines for Cancer Treatment
Cancers can be treated with a range of different treatment strategies, including radiation therapy, cytoreductive surgery, chemotherapy, and immunotherapy. Each has varying success from patient to patient.1
Incorporating nano-formulations into these treatments can improve their efficacy.2 In photothermal therapy, for example, nanoparticles help to localize heat and/or radiation, targeting tumors and reducing their resistance to treatment.
Therapeutic Delivery of Nanoparticles
Direct and systematic strategies have been developed to deliver nanoparticles for tumor targeting. Both approaches have advantages and limitations.
In the direct approach, nanoparticles are usually delivered to solid tumors via intratumoral injection.3
This method localizes many nanoparticles within the tumor, benefiting treatment efficacy. However, their distribution is rarely uniform. Within the tumor microenvironment, nanoparticles tend to cluster unevenly, creating pockets of high and low concentration. This irregular spread limits their overall effectiveness.
This unfavorable distribution results in a dense extracellular matrix in the tumor microenvironment that inhibits nanoparticle diffusion. To overcome this, systemic delivery methods, where nanoparticles are administered via the bloodstream, are being explored. These approaches have shown encouraging results in preclinical and clinical studies.
However, systemic delivery introduces its own set of challenges. Nanoparticles must survive a complex journey: navigating circulation, accumulating in tumour tissue, diffusing through dense tumour architecture, entering cancer cells, and releasing their drug payload. Along the way, they face biological interference.
A significant obstacle is the formation of a protein corona, when blood proteins bind to the nanoparticle surface after injection. This alters the nanoparticle’s physicochemical properties and can disrupt its intended function.
Opsonins, a class of proteins commonly deposited on nanoparticles, are problematic as they can trigger phagocytosis in macrophages. This can result in the removal of therapeutic nanoparticles from the bloodstream, stopping them from targeting tumors.
Several strategies have been developed to counteract these therapeutic barriers, such as coating nanoparticle surfaces with poly(ethylene glycol) (PEG).4
Nanoparticles Accumulate at the Target Sites
Many intravenously injected therapeutic nanoparticles are metabolized in the reticuloendothelial system (RES), accumulated in the liver or spleen, or cleared through the renal pathway.5 Any nanoparticles that avoid these processes will eventually accumulate in the tumor vasculature.
Once the nanoparticles have accumulated in this network of blood vessels, they can passively migrate to solid tumor tissue through leaky gap junctions between the endothelial cells lining the vasculature.6
Nanoparticles reach tumours through both passive and active mechanisms. They are passively absorbed via the enhanced permeability and retention effect. They can actively cross the vascular barrier through transendothelial pathways, where transcytosis enables transport across the vascular wall.
After all these processes occur, only a small fraction of the original nanoparticle dosage is endocytosed into tumor cells, causing cell death.
Endothelial cells in tumors differ from normal vascular endothelial cells in terms of cell proliferation, gene expression, migration ability, and response to growth factors and drugs.
Research has shown that tumor-associated endothelial cells have a higher active transportation capacity than normal cells due to an increased cellular proliferation rate.
Cellular Uptake of Nanoparticles
Nanoparticles travel into cells in a process called internalization. This is a highly regulated process mediated by endocytosis, where cells internalize extracellular materials by engulfing them within membrane-bound vesicles.7
Depending on the type of therapeutic nanoparticles and tumor cells being targeted, different endocytosis processes occur, such as clathrin-mediated, caveolin-mediated endocytosis, and macropinocytosis.
In clathrin-mediated endocytosis, nanoparticles bind to cell membrane receptors to trigger the tumor cell internalization process. Receptors include low-density lipoprotein, transferrin, β2-adrenergic, and epidermal growth factor receptors.
Caveolin-dependent endocytosis is slightly different and shields the therapeutic agents from hydrolytic enzymes and lysosomal degradation. Macropinocytosis is a non-specific cellular uptake mechanism that engulfs materials by extending an actin-stabilized plasma membrane.
Cells without clathrin and caveolin receptors carry out CLIC/GEEC, Arf6, and RhoA-mediated endocytosis.
After cellular internalization occurs, nanoparticles are confined within a membrane-lined vesicle known as an endosome. These endosomes fuse with vesicles and transport their cargo to various cellular targets, such as the mitochondria, cytosol, nucleus, endoplasmic reticulum, and Golgi apparatus.
Download your PDF copy now!
Nanoparticles Release Therapeutic Payload Inside Tumor Cells
Once nanoparticles reach tumour cells, they release their therapeutic payload in response to specific stimuli, depending on their formulation. This targeted release maximizes therapeutic effect while minimizing damage to surrounding healthy tissue.
For instance, some react to changes in pH, temperature, and the enzymes present in a tumor microenvironment.8 pH-sensitive nanoparticles release their drug payload in the acidic environment of the tumor. This targeted release is designed to maximise therapeutic effect while minimising damage to surrounding healthy tissue.
Enzyme-sensitive therapeutic nanoparticles have shown considerable potential. They respond selectively to enzymes commonly overexpressed in the tumour microenvironment.
This therapeutic method has shown significant improvements in specificity and effectiveness in cancer treatment. Scientists have recently designed temperature-responsive nanoparticles using polymeric, nano gel, and organic or inorganic nanomaterials for the smart delivery of therapeutic agents.
References and Further Reading
- Baskar R, et al. Cancer and radiation therapy: current advances and future directions. Int J Med Sci. 2012;9(3):193-9. doi: 10.7150/ijms.3635.
- Chehelgerdi M, et al. Progressing nanotechnology to improve targeted cancer treatment: overcoming hurdles in its clinical implementation. Mol Cancer. 2023;22(1):169. doi: 10.1186/s12943-023-01865-0.
- Sheth V, et al. Strategies for Delivering Nanoparticles across Tumor Blood Vessels. Adv Funct Mater. 2021;31(8):2007363. doi: 10.1002/adfm.202007363.
- Suk JS, et al. PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv Drug Deliv Rev. 2016;99(Pt A):28-51. doi: 10.1016/j.addr.2015.09.012.
- Hoshyar N, et al. The effect of nanoparticle size on in vivo pharmacokinetics and cellular interaction. Nanomedicine (Lond). 2016;11(6):673-92. doi: 10.2217/nnm.16.5.
- Milligan JJ, Saha S. A Nanoparticle's Journey to the Tumor: Strategies to Overcome First-Pass Metabolism and Their Limitations. Cancers (Basel). 2022;14(7):1741. doi: 10.3390/cancers14071741.
- Behzadi S, et al. Cellular uptake of nanoparticles: journey inside the cell. Chem Soc Rev. 2017;46(14):4218-4244. doi: 10.1039/c6cs00636a.
- Zhu J, et al. Harnessing nanotechnology for cancer treatment. Front Bioeng Biotechnol. 2025;12:1514890. doi: 10.3389/fbioe.2024.1514890.
Disclaimer: The views expressed here are those of the author expressed in their private capacity and do not necessarily represent the views of AZoM.com Limited T/A AZoNetwork the owner and operator of this website. This disclaimer forms part of the Terms and conditions of use of this website.