Sep 19 2010
A new material could help surgeons more accurately locate breast cancers, reduce the need for second surgeries and minimize pre-surgical discomfort for patients. Microscopic gas-filled spheres of silica, a porous glass, can mark the location of early-stage tumors to show their position using ultrasound imaging in the operating room.
A team of chemists, radiologists and surgeons at the University of California, San Diego, created the new material, which they describe in a forthcoming issue of the journal MedChemComm.
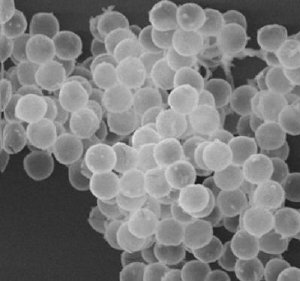 A scanning electron micrograph of porous silica microspheres filled with perfluoropentane vapor. This new material, invented at the University of California -- San Diego, is visible with Doppler ultrasound, sticks to breast tissue and can mark the location of tumors too small to be seen or felt during surgery. Credit: Paul Martinez, UCSD
A scanning electron micrograph of porous silica microspheres filled with perfluoropentane vapor. This new material, invented at the University of California -- San Diego, is visible with Doppler ultrasound, sticks to breast tissue and can mark the location of tumors too small to be seen or felt during surgery. Credit: Paul Martinez, UCSD
The X-rays used to make mammograms reveal calcium deposits associated with breast cancer even in tumors too small to be felt. But surgeons can't use X-rays while operating. Instead, radiologists place guide wires into tumors hours or even the day before surgery. The wires don't mark depth well and can shift. Patients find them both uncomfortable and unsettling.
As an alternative, the researchers created spheres of silica and filled them with perfluoropentane, a gas that has been used before in short-lived contrast materials for medical imaging. The rigid silica shells help the new material last longer.
"These little gas-filled microbubbles stick to human breast tissue for days and can be seen with ultrasound," said William Trogler, professor chemistry. "If doctors placed them in early stage breast cancer, which is difficult to see during surgery, they could help surgeons remove all of it in the first operation."
In the past few years, radiologists have tried implanting radioactive "seeds" instead of wires to mark tumors, but the seeds last only a few hours and must be inserted with a large-bore needle, which is painful. In addition, only one abnormal region can be marked, but patients with a form of breast cancer called ductal in situ carcinoma often have several. The seeds also expose both patient and staff to radiation, can't been imaged in three dimensions and create radioactive medical waste.
At just two micrometers in diameter – half the width of a strand of spider silk – small silica microbubbles can be precisely injected into clusters of abnormal cells using a thin needle. Radiologists would be able to inject the durable material days before surgery. And ultrasound scans reveal the position of the bubble in three dimensions on the operating table.
"Instead of just using a Geiger-counterlike device to say you're getting closer to the radioactive seed, you could actually see where to carve," said Andrew Kummel, professor of chemistry. The increased precision should help surgeons avoid the need for second surgeries.
"By outlining the tumor more completely in multiple directions, the particles could potentially help surgeons remove non-palpable tumors in a single operation," said Sarah Blair, a surgeon at Moores UCSD Cancer Center. "They will definitely make the operation more comfortable for patients."
The researchers think the ultrasound pressure waves burst the microbubbles. "They're thin, fragile balls of porous glass, like Christmas tree ornaments," Kummel said. "The shell is just one two-hundredth of the diameter of the ball. When it breaks, the gas squirts out. Doppler ultrasound detects that movement."
Nano-scale silica microbubbles, which the team reports in this paper as well, are too small to remain in place, but might drain from a cancerous site to help identify which lymph nodes are most likely to contain stray cells that could help the cancer spread.
The current study demonstrates the feasibility of the technology in tissue samples. Tests in animal models are underway, and toxicology studies must also be completed before clinical trials in humans could begin.
Chemists Bill Trogler, and Andy Kummel, of UCSD's Division of Physical Sciences, and radiologist Robert Mattrey and surgeon Sarah Blair of the Moores UCSD Cancer Center led the project. Additional co-authors include radiologist Yuko Kono, and Sergio Sandoval, Moores UCSD Cancer Center; Paul Martinez of the Department of Chemistry and Biochemistry; and Jessica Wang-Rodriguez of the Department of Pathology.
The National Cancer Institute provided financial support for this study.