Apr 5 2017
 Credit: Oregon State University
Credit: Oregon State University
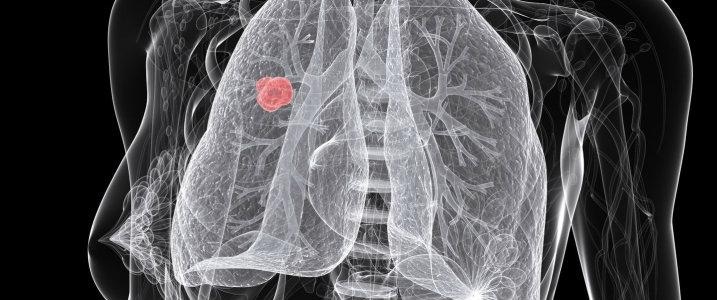
An innovative cancer-drug delivery system has demonstrated the potential to utilize the oxygen-deficient regions of solid tumors that render the growths to be immune to standard radiation and chemotherapy treatment.
Solid-tumor cancers include carcinomas affecting the colon, breast, prostate, and lung, as well as malignancies in the lymphatic system (called lymphomas), and the very less common sarcomas occurring in the connective tissue.
Such solid masses usually comprise of hypoxic regions in which the oxygen concentration in the tissue is very low. The growth of hypoxic cancer cells is very slow, rendering them less vulnerable to the drugs formulated to destroy or damage such cells.
Scientists from the Oregon State University (OSU) have developed an innovative technique to reverse the nature of these cells by loading a “prodrug” into nanostructured platforms.
A prodrug is a kind of pharmacologically inactive compound metabolized by the body into an active drug; here, the compound is vinblastine, a cancer drug.
Research collaborators from Cascade Prodrug Inc. of Eugene, Oregon, offered the vinblastine-N-oxide prodrug to the OSU scientists, who used it to create two varied lipid-based platform formulations called liposomes to transfer the prodrug to the hypoxic areas of the tumor. The oxygen deficiency in those areas activates the metabolic conversion of the prodrug into vinblastine.
One of the formulations included polyethylene glycol on its surface, and the other did not. The prodrug was seen to be safe as well as highly effective on non-small cell lung cancer in both the formulations when compared to delivering it without a liposome.
One of the hallmarks of these solid tumors is their hypoxic regions. One reason these cancers become very aggressive is the development of this hypoxia. Since the late 1990s, researchers have been trying to take advantage of the hypoxia. The tumor model we chose, lung cancer, is one of the very well established tumors and there’s a very strong hypoxia associated with that—as well as, lung cancer is one of these cancers that in its advanced stages, it’s a terminal disease, and there’s a need for new treatments.
Adam Alani, OSU College of Pharmacy
When vinblastine-N-oxide was administered as such, it demonstrated an efficiency that was less than optimal when tested by Cascade Prodrug. This is due to the fast manner in which the body clears the drug from the system, that is, the drug has a half-life of less than 30 minutes.
“When it was tested in mice and dogs, it did not have a chance to assimilate in the cancer tissue to produce the desired pharmacological effect,” stated Alani.
However, both the “pegylated” liposome including polyethylene glycol and the non-pegylated liposome drastically increased the half-life to 9.5 and 5.5 hours, respectively.
The nano carriers performed much better than the prodrug itself. We were able to literally cure the tumor.
Adam Alani, OSU College of Pharmacy
Laboratory cultures were the initial step of Alani’s study that gradually advanced to efficacy and safety testing in animals.
“We made sure the nanostructure platform worked properly against lung cancer in vitro, then looked at the safety of the formulation in healthy mice and looked at the maximum tolerated dose—the biggest dose you can use without producing side effects,” stated Alani. “Then we determined how long the nano carriers could keep the drug in the blood compared to the drug without the nanostructures.”
As the data were found to be “very encouraging,” Alani’s and his colleagues evaluated the efficacy of the liposomes in mice into which tumors had been grafted.
When both the liposomes were not used, the drug was found to somewhat suppress tumor. However, the mice to which only the drug was administered had to be euthanized after 70 days as the tumors started to grow uncontrolled.
Mice to which the drug was administered using either of the liposomes were found to be tumor-free and healthy for 100 days duration of the experiment.
The formulations clearly performed better than the unformulated drug as well as much better than Cisplatin, the standard-of-care drug for this research. Now we’re collaborating with Cascade Prodrug and the College of Veterinary Medicine to assess safety and efficacy in dog models, and trying to look at other tumors, like bladder cancer, associated with dogs.
Adam Alani, OSU College of Pharmacy
According to Alani, one aim was to create an innovative treatment for cancer in dogs, and the other aim is to use dogs as a model for developing drugs—“to get data Cascade can use to move the process forward for approval for use in dogs, as well as preliminary data for a new drug application with the FDA,” stated Alani.
The study was supported by the Oregon Nanoscience and Microtechnologies Institute. The outcomes of the study were recently reported in the Journal of Controlled Release.
Alani’s collaborators in the Department of Pharmaceutical Sciences, Vidhi Shah, Duc Nguyen, and Adel Alfatease, as well as Shay Bracha from the OSU veterinary college’s Department of Clinical Sciences were the co-authors of the paper.