The article aimed to further the field of regenerative medicine and tissue engineering through nanotechnology incorporation using a novel biomaterial.
The Importance of Bone Tissue Engineering
Bone tissue engineering (BTE) focuses on increasing bone regeneration and repair through the synthesis of substitutions to conventional bone grafting materials.
This is significant due to the clinical applications in different areas of medicine, for transplants as well as for including dentistry through socket preservation, alveolar ridge augmentation, as well as guided bone regeneration.
Natural bone found within the body is consists of a non-mineralized organic component that is mainly type-1 collagen as well as a mineralized inorganic component, such as carbonated apatite minerals.
The challenge of bone tissue engineering is having the ideal scaffold, that should be analogous to the natural bone as well as provide the optimum microenvironment that ensures cell growth.
The composition of these materials requires an alteration to imitate natural bone, with macromolecules being used as organic substrates and hydroxyapatite (HA) being used for the inorganic substrate; these components are mixed within suitable proportions to imitate the ratio of the organic and inorganic composition of natural bone tissue.
This matching and imitation to native bone tissue are considered to be one of the most challenging aspects of bone tissue engineering, with a lack of natural interaction with native tissue as well as having poor mechanical properties to serve clinical applications effectively.
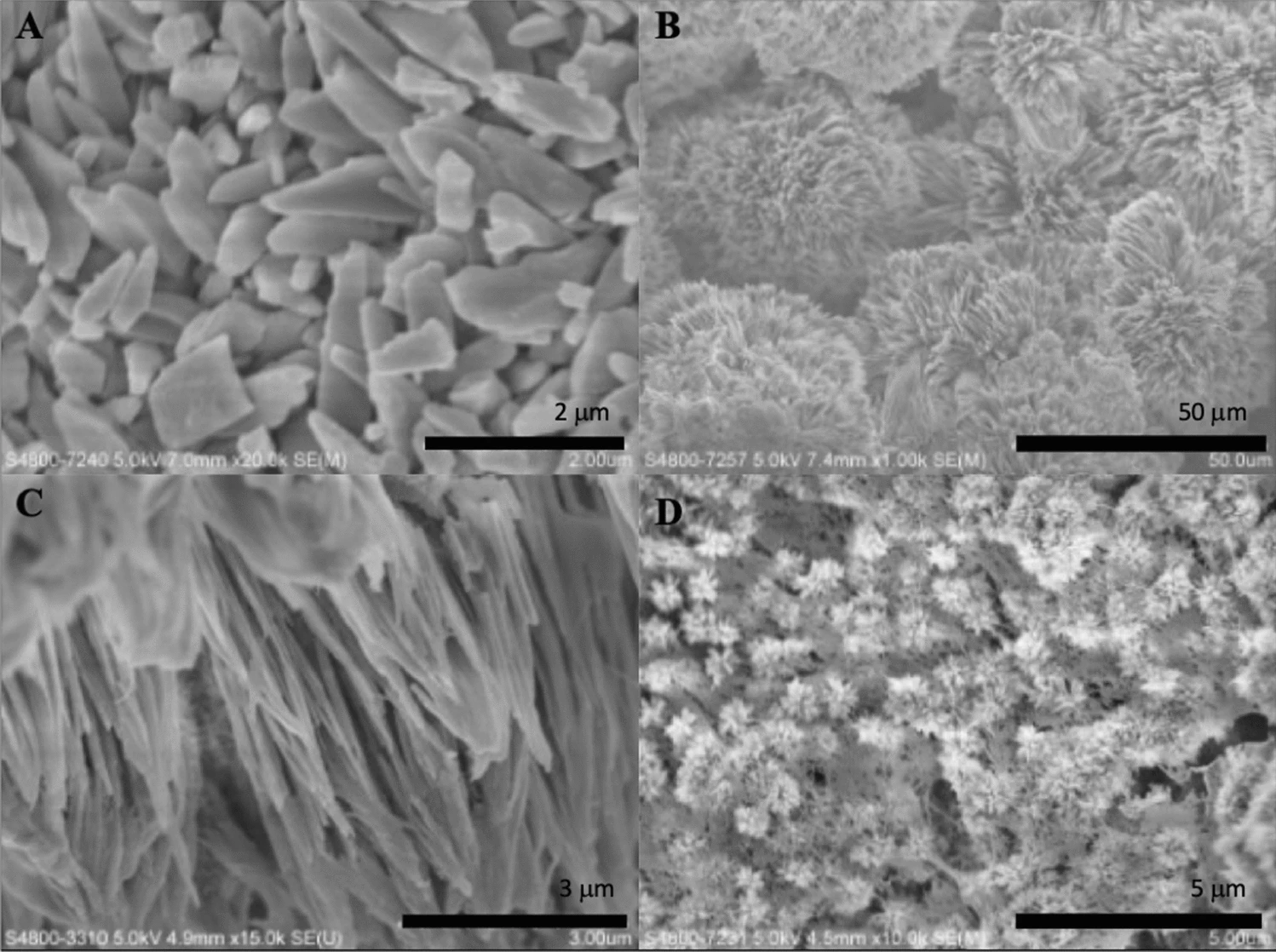
Figure 1. SEM micrographs of formed crystals treated with different strength of electric current. (A) 5 mA; (B) 8 mA; (C) 10 mA; (D) 12 mA. © Khosalim, I., Zhang, Y., Yiu, C. and Wong, H., (2022)
Challenges of BTE Materials
Natural, synthetic, bioceramic and metal materials have previously been used in BTE, however, their limitations can prove to be a challenge for clinical applications.
Natural materials consist of collagen, chitosan, and alginate; however, their weak mechanical properties and fast degradation illustrate their limitation for the formation of hard tissue.
Synthetic materials can include polycaprolactone, polylactic acid and polyglycolic acid, which releases acidic products during the degradation process, resulting in the unfortunate formation of tissue necrosis.
Bioceramic materials comprise calcium phosphate bioceramic, hydroxyapatite, β-tricalcium phosphate, and bioactive glass.
These materials have drawbacks such as being challenging to shape due to being extremely brittle, stiff, as well as having low flexibility and poor molding properties. This adds to the profile of these materials being mechanically weak.
Other BTE materials include metals such as titanium and magnesium and their associated alloys which lack the potential for drug delivery applications. Apart from magnesium and its alloys, these materials do not degrade.
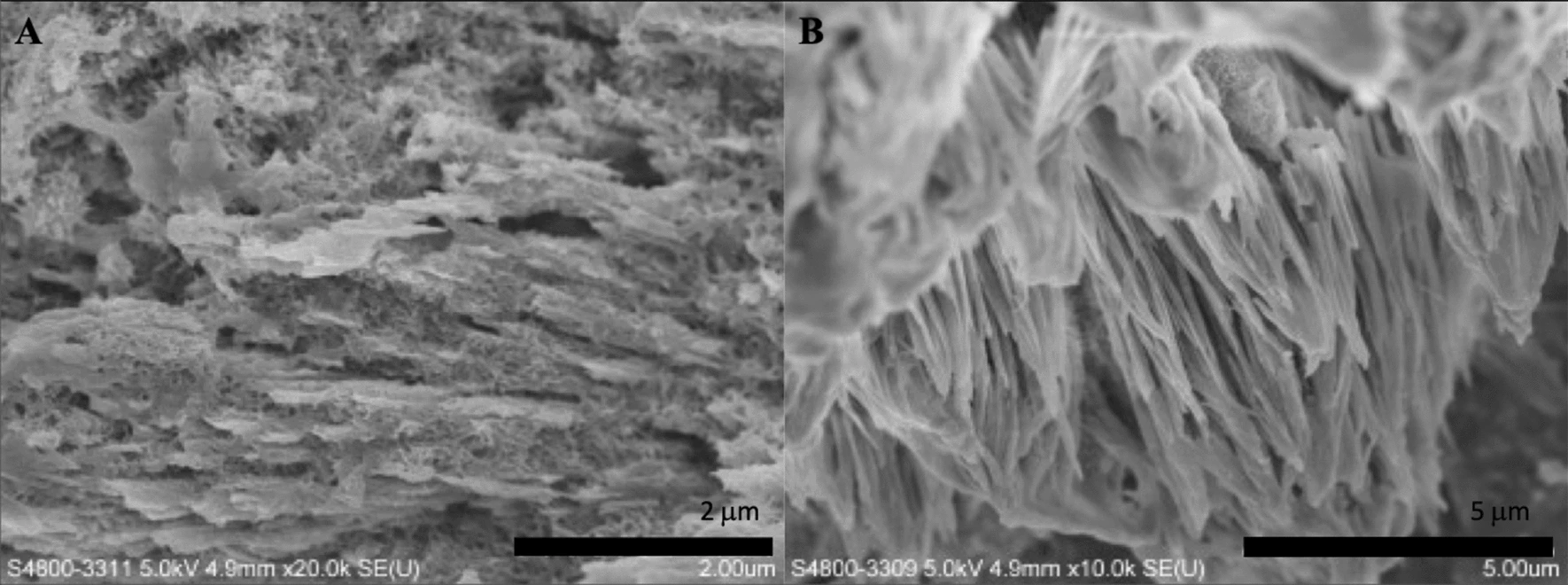
Figure 2. SEM micrographs of the synthesized biomaterial treated with a current of 10 mA, after 10 h mineralization. (A 20.0 k × magnification; B 10.0 k × magnification). © Khosalim, I., Zhang, Y., Yiu, C. and Wong, H., (2022)
Novel Biomaterial BTE Candidates
The potential of using the novel biomaterial, graphene to advance this field of bone tissue engineering, can be significant. Graphene materials have demonstrated benefits for clinical use through having high mechanical strength, elasticity and flexibility.
The further use of graphene oxide (GO), the oxidized form of graphene, which retains many hydrophilic functional groups, including hydroxyl and carbon groups, can work effectively in aqueous solutions due to high dispersibility, as well as binding efficiently with metal ions and nanoparticles.
Additionally, the affinity of GO for antibacterial activity can also prove to be an effective component for bone tissue engineering as a strategy to control and prevent infection, and this has been evidenced by previous studies.
The researchers of this study combined the use of GO, with agarose (AG), a natural polymer that is biodegradable and demonstrates similarity to bone extracellular matrix.
The use of this natural polysaccharide can aid in the formation of a gel network that allows diffusion and the transport of oxygen and nutrients within the scaffold.
The addition of hydroxyapatite, a bioactive inorganic ceramic, to this BTE combination, also has the potential to create an effective scaffold due to this component having chemical and crystallography that is similar to natural apatite found in native bone tissue.
While this material is brittle on its own, it works well with other materials and has its own advantages such as cell adhesion and good osteogenic activity.
The triple component of GO, AG and HA is novel for use as a bone tissue scaffold material; the researchers presented this combination through a low-cost and simple electrophoresis system to produce biomaterials.
The method of electrophoresis consists of ion migration in a specific one-dimensional direction, which can transport ions fast through gel or solutions compared to diffusion alone.
This method was used to accelerate HA formation in agarose hydrogels for producing this triple component hybrid material.
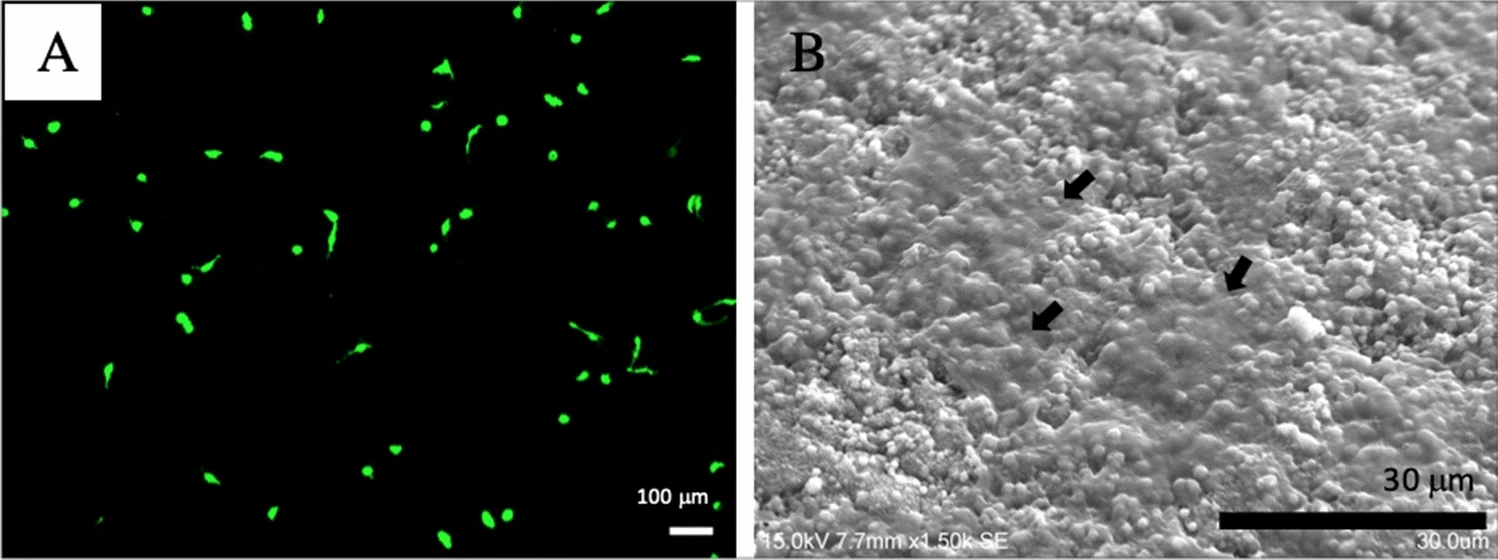
Figure 3. MC3T3-E1 cultured on synthesized biomaterial after 3 days on (A) LCSM; (B) SEM, with the arrows represent attached MC3T3-E1 cells. © Khosalim, I., Zhang, Y., Yiu, C. and Wong, H., (2022)
Future Translation
The potential of this research can be revolutionary for not only the field of bone tissue engineering but regenerative medicine as a whole, due to widespread clinical applications for which this research can be used.
The triple component hybrid scaffold material also demonstrated safety with cell viability assays as well as high antibacterial activity with results of reduced Staphylococcus aureus being found, further illustrating its potential for use within BTE.
The synthesis of biomaterials in this novel electrophoresis method was proven to be promising and with cost-effective and simple strategies. This method has the potential to be utilized for all industries from electronics to medicine.
Reference
Khosalim, I., Zhang, Y., Yiu, C. and Wong, H., (2022) Synthesis of a graphene oxide/agarose/hydroxyapatite biomaterial with the evaluation of antibacterial activity and initial cell attachment. Scientific Reports, 12(1). Available at: https://www.nature.com/articles/s41598-022-06020-1
Further Reading
Black, C., Goriainov, V., Gibbs, D., Kanczler, J., Tare, R. and Oreffo, R., (2015) Bone Tissue Engineering. Current Molecular Biology Reports, 1(3), pp.132-140. Available at: https://doi.org/10.1007/s40610-015-0022-2
Disclaimer: The views expressed here are those of the author expressed in their private capacity and do not necessarily represent the views of AZoM.com Limited T/A AZoNetwork the owner and operator of this website. This disclaimer forms part of the Terms and conditions of use of this website.