Mar 3 2008
A team from UCL has developed a new medical device which will make the early detection of breast cancer more cost effective and easier to administer. The team - which won a prestigious Brian Mercer Feasibility Award from the Royal Society yesterday - plans to use magnetic nanoparticles and an extremely sensitive magnetometer called the ‘HistoMag’ to detect cancerous cells in samples of breast tissue.
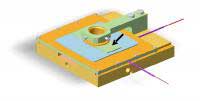 Schematic of the HistoMag magnetic microscope. The arrow points to a glass slide for mounting biopsy tissue.
Schematic of the HistoMag magnetic microscope. The arrow points to a glass slide for mounting biopsy tissue.
“Each year 35,000 women are diagnosed with breast cancer in the UK and the testing programme is a massive undertaking,” says Professor Quentin Pankhurst of the London Centre for Nanotechnology and the UCL Department of Physics & Astronomy. “Until now, pathologists had to stain tissue samples with brown dyes to help them determine whether they were normal or cancerous. In terms of streamlining the process, the main problem is that all of the results are open to interpretation and each test has to be individually checked by a specialist.
“At UCL we’ve been working in the relatively new area of biomagnetics to develop a technique which provides more quantitative and reliable results, whilst also enabling pathologists to identify abnormal tissue sections much more quickly.
“Cancerous cells have a protein on their surface called HER2. We use a solution of HER2 antibodies, tagged with magnetic nanoparticles, to stain the tissue sample. Using the HistoMag we can detect the quantity of tagged antibodies which attach themselves to the HER2 protein, which in turn provides us with an accurate picture of the spread of cancerous cells.”
By automating the process through which cancerous cells are detected and quantified, HistoMag will not only ease the pressure on pathologists but also help to identify the 15-30% of patients who are likely to benefit from being treated with the drug Herceptin. At a cost of £30,000 per patient per annum it is essential to target Herceptin at those women who will respond positively to it.
The team, led by Professor Pankhurst, is one of only seven groups to receive a Brian Mercer Feasibility Award from the Royal Society this year. The £25,000 award will enable the team to re-engineer the HistoMag, increasing its sensitivity before it goes on to clinical trials. Their goal is to make the device generally available to pathologists in 2010.