A global team of researchers has reversed Alzherimer's symptoms in mice using just three nanoparticle injections, restoring brain function by repairing the blood-brain barrier.
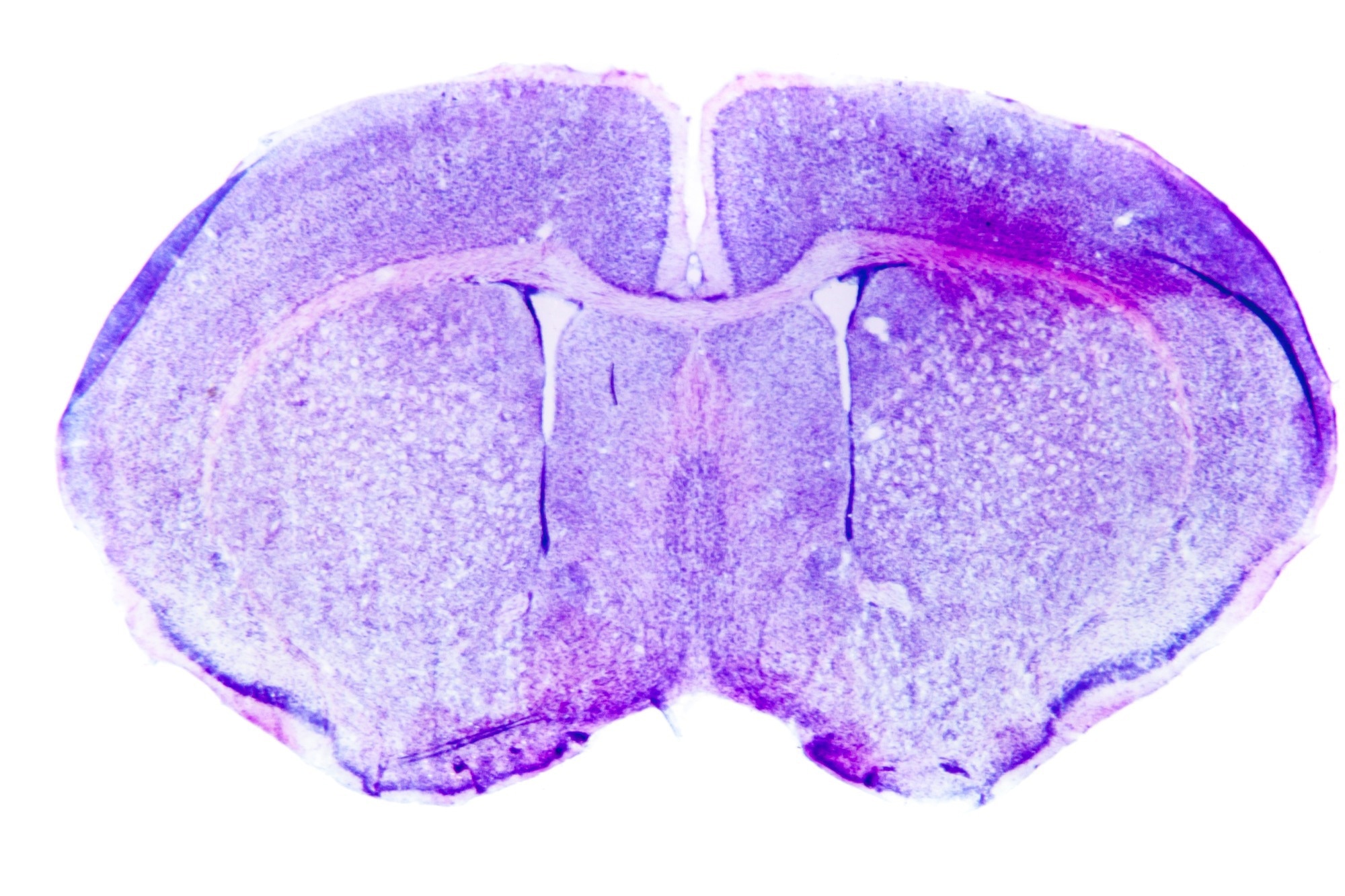 Image Credit: Pan Xunbin/Shutterstock.com
Image Credit: Pan Xunbin/Shutterstock.com
This groundbreaking method developed by the Institute for Bioengineering of Catalonia (IBEC) and the West China Hospital Sichuan University (WCHSU) addresses the disease by restoration of normal vascular function, rather than targeting neurons or other brain cells, which has been the conventional approach until now.
Unlike most nanomedicines, which use nanoparticles as carriers for therapeutic agents, this method employs nanoparticles that possess bioactive properties, often known as "supramolecular drugs."
Rather than directly targeting neurons, the therapy aims to restore the proper functioning of the blood-brain barrier (BBB), which is the vascular gatekeeper regulating the brain’s environment. By mending this essential interface, the researchers successfully reversed Alzheimer’s pathology in animal models.
The brain is the most energy-intensive organ in the body, using 20 % of the energy in adults and as much as 60 % in children. This energy is delivered via an extensive blood supply supported by a distinctive and dense vascular network, where each neuron is supplied by a single capillary.
The brain is home to around one billion capillaries, underscoring the essential function of brain vasculature in preserving health and fighting disease. These observations emphasize the importance of vascular health, particularly in conditions such as dementia and Alzheimer’s, where a weakened vascular system is closely associated.
The BBB serves as a cellular and physiological barrier that distinguishes the brain from the bloodstream, safeguarding it against external threats such as pathogens and toxins.
The research team demonstrated that targeting a specific mechanism makes it possible to facilitate the passage of unwanted "waste proteins" generated in the brain through this barrier, allowing for their removal via the bloodstream. In the context of Alzheimer’s disease, the primary "waste" protein is amyloid-β (Aβ), whose buildup disrupts the normal operation of neurons.
The researchers used mouse models genetically engineered to produce elevated levels of Aβ protein, resulting in significant cognitive decline that resembles Alzheimer’s pathology. After administering only three doses of the supramolecular drugs, they regularly monitored the disease's progression.
Only one hour after the injection we observed a reduction of 50-60 % in Aβ amount inside the brain.
Junyang Chen, Study First Co-Author and Researcher, West China Hospital of Sichuan University
The most remarkable findings were the therapeutic effects. Researchers carried out a series of experiments to examine the animals' behavior and assess their memory deterioration over several months, encompassing all phases of the disease.
In one experiment, they administered nanoparticles to a 12-month-old mouse (analogous to a 60-year-old human) and evaluated its behavior after six months. The outcome was striking: the mouse, previously engineered to have poor brain health, was now 18 months old (equivalent to a 90-year-old human), and showing behavior characteristics of a healthy mouse.
The long-term effect comes from restoring the brain’s vasculature. We think it works like a cascade: when toxic species such as amyloid-beta (Aβ) accumulate, disease progresses. But once the vasculature is able to function again, it starts clearing Aβ and other harmful molecules, allowing the whole system to recover its balance.
What’s remarkable is that our nanoparticles act as a drug and seem to activate a feedback mechanism that brings this clearance pathway back to normal levels.
Giuseppe Battaglia, ICREA Research Professor, Institute for Bioengineering of Catalonia
Amyloid-Β Clearance from the Brain
In Alzheimer’s disease, a significant issue is that the brain’s inherent clearance mechanism for toxic substances such as amyloid-β ceases to function effectively. Typically, the protein LRP1 serves as a molecular gatekeeper: it identifies Aβ, attaches to it via ligands, and transports it across the blood-brain barrier into the bloodstream for removal.
This system is delicate. If LRP1 binds excessively to Aβ with too much affinity, the transport becomes obstructed, and the protein itself is degraded within the brain barrier cells, resulting in a reduced number of available LRP1 "carriers." Conversely, if it binds insufficiently, the signal is too weak to activate transport. In both scenarios, the outcome is identical: Aβ accumulates within the brain.
The supramolecular drugs developed in this research function as a switch that reboots the system. By imitating the ligands of LRP1, they can attach to Aβ, traverse the blood-brain barrier, and commence the removal of toxic substances from the brain. In this manner, they assist in restoring the vasculature’s natural function as a waste-clearing pathway, returning it to its proper operation.
Nanoparticles to Treat Alzheimer’s
The scientists presented nanoparticles that function as supramolecular drugs, serving as therapeutic agents independently rather than merely as medication carriers.
These nanoparticles feature precise size regulation along with a specific number of surface ligands, forming a multivalent platform engineered using a bottom-up molecular approach capable of interacting with cellular receptors in a highly targeted manner.
The team provides a distinctive and innovative method to modulate receptor activity by influencing receptor trafficking at the cell membrane. This level of precision not only facilitates the efficient removal of amyloid-β from the brain but also reinstates equilibrium in the vascular system that supports optimal brain function.
This groundbreaking therapeutic approach presents a hopeful avenue for creating effective clinical interventions, tackling vascular factors related to Alzheimer’s disease, and ultimately improving patient outcomes.
Our study demonstrated remarkable efficacy in achieving rapid Aβ clearance, restoring healthy function in the blood–brain barrier and leading to a striking reversal of Alzheimer’s pathology.
Lorena Ruiz Perez, Researcher, Molecular Bionics Group, Institute for Bioengineering of Catalonia (IBEC) and Serra Hunter Assistant Professor, Faculty of Physics, University of Barcelona (UB)
The study was conducted in partnership with the Institute for Bioengineering of Catalunya (IBEC), West China Hospital of Sichuan University, West China Xiamen Hospital of Sichuan University, University College London, the Xiamen Key Laboratory of Psychoradiology and Neuromodulation, University of Barcelona, the Chinese Academy of Medical Sciences, and the Catalan Institution for Research and Advanced Studies (ICREA).
Journal Reference
Chen, J., et al. (2025) Rapid amyloid-β clearance and cognitive recovery through multivalent modulation of blood–brain barrier transport. Signal Transduction and Targeted Therapy. doi.org/10.1038/s41392-025-02426-1